Image-guided therapy
Image-guided surgery uses medical scans, computing and tracking to make treatment more efficient and less invasive and less riskful for the patient. Parts of Image-guided therapy include image- guided radiotherapy and image-guided surgery.
For a general description of imaging techniques, please have a look at the article Brain Tumor Diagnosis.
Intraoperative Imaging
Intraoperative images are used as additional information for the surgeon to detect changes during surgery. Different imaging modalities are in use in today's intraoperative imaging.
Overview over modalities
MRI: Intraoperative MRI images can be produced using different devices, where most of them work in a low-field spectrum. In a special purpose horizontal bore 0.5 T superconducting magnet system, the patient lays inside a double donut. This system gives only little constraints to the access to the patient. Similar impacts hold for general purpose 0.2/0.3 T permanent or electro-magnet systems. In one of this systems, pole-pieces are integrated into the OR table and the field can be raised when needed. In contrast to these systems, conventional 1.5 T systems can be used in the OR as well. These show better quality in the resulting images due to a stronger filed. However, images can only be taken between surgical steps because the patient has to be put inside the magnet. So for the use of MRI, the surgeon has to weight the trade-off between image quality and extra time and effort for producing the images. In general, magentic fields in the OR can introduce a potentially unsafe environment. Further steps indicate the integration of MRI imaging with surgical robotics. [3]
CT: Intraoperative CT scanning takes place with the help of a C-arm. These devices make it possible to take CT images during surgery without moving the patient to another area of the OR room, as for MRI scans. These CT scans can then be compared to pre-operative ones to posibbly adjust the surgical procedure.
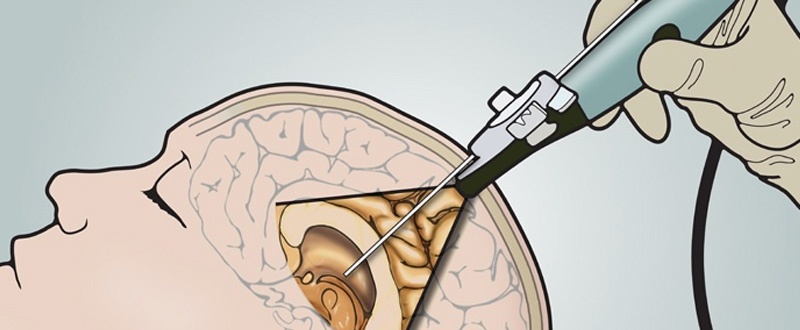
Ultrasound: Ultrasound is commonly used for intraoperative imaging because it is cheap and enhances minimal risks. It can detect changes in the patients brain and update pre-operative CT/MRI images. However the ultrasound transducer has to be in direct contact with the brain tissue, which can restrict the work of the surgeon. [3]
Fluoroscopy:A sequence of X-ray scans can be used to see movement of for example the blood vessels inside the brain. By using a mobile system, the scans can be taken without moving the patient during surgery.
Figure 6: schematic of intraoperative Ultrasound [17]
Research on intraoperative MRI
Brain shift describes the deformation of the brain due to surgical practices. After brain-shift, the preoperative images don't resemble reality anymore. So if the surgeon works with reference to the preoperative scans, e.g. during tumor resection, he could miss tumor tissue and cut out healthy brain tissue. Intraoperative MRI imaging is used to incorporate this shift. In one method, the intraoperative MRI images are combined to a 3D model and registered with the help of bone fiducial markers attached to the head. Afterwards the new images are combined with the preoperative images in a neuronavigation system, which was updated acording to the difference between both images. Results from this trial show that the use of intraoperative MRI images led to a total resection of the tumor in 14/16 tumors. In the two other patients, the tumor grew into sensitive brain tissue, so that it was partly inoperable. So this system shows a reliable navigation with high accuracy, compared to a system without measuring the brain shift through MRI images. [13]
Image Registration/Image Fusion
Overview
Image registration (i.e. geometric alignment) is the process of registering preoperative images and intraoperative images into the same reference frame (i.e. registration of a virtual patient and a real patient). During registration, data sets from different planes, different times (serial registration), different imaging modalities (multi-modal registration), one patient (intra-subject) or multiple patients (inter-subject) are spatially matched. This allows the combination and refinement of anatomical, functional and metabolic imaging. [9] [11]
Rigid image registration uses landmarks. Because many parts of the anatomy are constantly moving, finding fixed landmarks is troublesome. Fiducial markers address this problem: they can be added either on the skin – and may move with the skin – or directly on the bone. The markers can then be found in the preoperative and the intraoperative images and both image types can be combined. Rigid image registration can be applied when the images that are to be matched only differ in rotation and translation. [9]
Usually, registration is complicated by the anatomical changes during the surgery and regular deformations of the anatomy (e.g. because of breathing). Non-rigid registration aims at these deformations by stretching and warping the preoperative image to the intraoperative image. [9] There was a lot of research during the last years in non-rigid registration, but currently they lack the robustness for clinical practice. [10]
Image registration
Image registration means finding the optimal geometric transformation that maximizes the correspondences between two images. Rigid and non-rigid algorithms consist of the following three main components:
- Transformation model: the transformation model defines transformation between the images. In case of a rigid registration, it only performs rotation, translation and scaling (i.e. linear transform). In case of a non-rigid registration, every location pixel/voxel is moved to the transformed location by a displacement vector field (i.e. not a linear transform). Non-rigid registrations are usually smooth and invertible, resulting in non-collapsing structures within the image model. That means that the size and shape changes, but not the topology. In surgery, this is not the case and would need an other approach. For non-rigid registrations, there are parametric and non-parametric models. In parametric models , the displacement vector field for all image points is associated with one discrete 3D grid. Therefore the displacement is a general displacement to a specific location. In non-parametric models, the displacement vector is calculated for each voxel.
- Similarity metric: the similarity metric measures the degree of alignment between images. Intensity-based registration and feature based registration are the two main methods. Intensity-based registration is the main method in rigid registration and compares image intensities to measure alignment. Feature-based registration is better for multi-modal registration and measures the distances between specific features (especially landmarks).
- Optimization method: the optimization method maximizes the similarity metric using numerical methods.
Further readings
Here, we listed some papers that might be interesting for further reading/discussion, but which we were not able to review due to time limitations.
Bibliography
[1] https://med.nyu.edu/neurosurgery/physicians/a-z-technologies-guide/image-guided-surgery
[7]Nam P. Nguyen, Mai L. Nguyen, Jacqueline Vock, Claire Lemanski, Christine Kerr, Vincent Vinh-Hung, Alexander Chi, Rihan Khan, William Woods, Gabor Altdorfer, Mark D’Andrea, Ulf Karlsson, Russ Hamilton and Fred Ampil Potential Applications of Imaging and Image-Guided Radiotherapy for Brain Metastases and Glioblastoma to Improve Patient Quality of Life; published in frontiers in oncology (2013); DOI: 10.3389/fonc.2013.00284
[13] Christopher Nimsky, M.D., Oliver Ganslandt, M.D., Peter Hastreiter, Ph.D., and Rudolf Fahlbusch, M.D.; Intraoperative Compensation for Brain Shift; published in Surgical Neurology (2001); DOI: 10.1016/S0090-3019(01)00628-0
[15] https://healthmanagement.org/c/imaging/news/intraoperative-mri-success-at-tubingen-hospital
[17] http://blog.bkultrasound.com/advantages-of-ultrasound-over-mri-or-ct-in-neurosurgery
[18] http://realspinesurgery.com/spine-surgery/#intraoperative-fluoroscopy








2 Kommentare
Unbekannter Benutzer (ga83mor) sagt:
06. Juni 2017Feedback from group 2. Good job guys, well structured and easy to read. I was really pleased to see the #Further readings. The only thing I would say I am not sure that it was worth to write about image registration, because it is really a huge and non trivial topic and a few paragraphs is definitely not enough.
Unbekannter Benutzer (ga67yur) sagt:
07. Juni 2017Thanks for the feedback!