Intraoperative Imaging
Intraoperative MRI (iMRI/ioMRI)
The first interoperative setup for MRI imaging has been developed at the Magnetic Resonance Therapy (MRT) Unit at Brigham and Women's Hospital (BWH) in Boston, Massachusetts. Driven by the need to have up-to-date images during the procedure the "double-douhgnut" shape of the system allowed surgeons to access the patient during the operation while minimizing the effort to acquire images of the brain interoperatively. During this initial phase, not only the appliance itself needed to be adapted to the new use, also the instruments used in the operation room had to be revised, to minimize the interference with the the device and to avoid artefacts on the scans.
Since then the technology has made tremendous advances, creating a variety of set-ups, which meet different requirements of iMRIs. A downside of the initial setup, is the narrow space for the surgeon between the two parts of the device. This problem was overcome be the development of other open-configuration MRIs which however use weaker magnets (~0.2-0.5T) and therefore can only provide a lower image quality. The second option is a portable device, which is stored in an adjacent room when not in use. The stronger magnets (1.5 -3T) allow for higher image resolution with the downside of a longer set up time and therefore a prolonged operation time. This is also referred to as closed configuration [1][2].
An open configuration ("double-doughnut") MRI device. The surgeons can access the patient in the gap between the two rings. The patient himself does not need to be moved during the image acquisition [3].
(above) A modern mobile closed-configuration MRI scanner. The device is mounted on rails on the ceiling of the operation theatre. When needed, it can be moved into the room and "docked" onto a specialized operation table. (below) Two operation rooms can share an MRI scanner, which can turn around its axis.
Intraoperative CT (iCT)
As in the case of mobile MRI scanners, intraoperative CT scanners can be installed in an operation room. Unlike iMRI, iCT does not need specialized operating equipements since there is no strong magnet, that may transform ferromagnetic objects into projectiles. Modern iCT aplliances are fully mobile and can be brought to any operating theatre upon request. The integration of the iCT scan into the operation is feasible with minor modifications of the general workflow but setup and imaging increase the operation time. Since CT is a fast procedure, depending on the surgery the preparation and imaging process can add up 15 minutes [6].
"Airo" is a modern fully mobile CT scanner, that can be used during the operation. It is sold by Brainlab, a technology enterprise specialized in software design for medical procedures. Setups of other providers may include a rail guided system [7].
Flourescence image-guided surgery (FIGS)
Major drawbacks of iCT and iMRI are the size and the costs of the devices, as well as the maintenance of such machines especially of the necessary sterile environment in the operation room. Another problem, that cannot be overcome by the above mentioned imaging methods is, that the boundaries of tumours are often diffuse and the previous methods often can only provide ambiguous imaging, especially when using low resolution devices. Fluorescence based imaging relies on the fact that certain agents accumulate in the tissue of interest and can than be excited using the appropriate wavelength.These can be detected using low-power surgical microscopes. In recent years this technique has been shown to improve the surgical quality [8][9][10].
There are several types of fluorescent agents:
- Passive agents: Some of the agents increase the permeability of the blood-brain barrier and can leak into the tumour tissue. However, this approach is not very specific due to the natural diffusion process.
- Metabolic agents: Are activated via a metabolic process. In the ideal case one should chose an agent, that targets a metabolic process, that is highly active in the tissue of interest. A current molecule of interest is 5-aminolevulinic acid (5-ALA) which is florescent in its activated form protopotphyrin IX (PpIX) [8].
- Molecular targets: Those agents are designed to specifically target a cell of interest via cell surface receptors. Remaining challenges include the distinction of specific from unspecific binding [10].
Intraoperative imaging
In practice, the use of interoperative imaging allows the surgeon to interactively asses his/her approach during the operation (e.g. rescanning the tumour after debulking of the tissue in order to remove as much of the aberrant tissue as possible. The shift of the brain during the operation can be assessed and the necessity of awake surgery decreases. The use of these techniques seemingly reduces the number of second procedures necessary [1][2]. The imaging techniques can be used to verify the outcome of the operation before the patient leaves the operation room, and adjustments can be made directly, for example the correction of shunt placement. Furthermore, it is hoped, that intraoperative imaging increases the accuracy of the procedures and prevent long-term return to the operation table [11].
Augmented Reality
Augmented Reality is being one of the trends that beside entertainment it is finding a broad use in medicine as well. It is a very promising technology and it is going to have a very important role in future medicine. Medical Augmented Reality makes use of glasses or other visual gadgets that can project different information (organs, images, patient’s data) into the real world. The projection happens in real time and the data projected must be very accurate and well registered to be usable. Hence, there are a lot of problems that are being faced, however, the technological trend is reaching very satisfying levels [12].
Some problems in the area of medical augmented reality are mainly concerned with registration and alignment of augmented information into the real world. The first problem is to register the data correctly as well as to show depth perception. It is not that straight forward as projecting some image into the skin, because the instruments and data from the real world will be invisible. There are techniques with opaque, shadows, ghosting, depth of perception etc. A very good example is from the study the CAMP Chair, for Focus & Context Visualization in Augmented Reality. Some images from the project on how the Augmentation of information into patient’s body is achieved is presented in the pictures below [13].
Augmented reality tool insertion into body [13]
Another area where Augmented Reality came in handy is in guided neurosurgery. According to a research, the accuracy and intraoperative application of an image projection technique in the form of Augmented Reality was really successful. The procedure consists of projection into patient’s head (skull) in order to guide through a tumor surgery. Images of the segmented brain tumor were generated and augmented into the patient’s head, which lead into a successful dissection of the tumor. Hence, it was concluded that the method is reliable and help significantly in planning neurosurgical procedures [14].
Augmented Reality for Neurosurgeons with Kinect and Brain Scans AR [15]
Furthermore, there is even a more promising path of Augmented Reality in Training and Planning of Brain Tumor Resection. Brain cancer is being considered as one of the least survivable type of cancer worldwide, hence, there is a need for more reliable and generally better techniques for diagnosis and planning. A very promising research considers Augmented Reality as one of the approaches against 2D images or even 3D reconstructions. The paper emphasizes the importance of accuracy and precision provided for planning brain tumors resection. It is foreseen that newer generations of surgeons have a better sense in capturing easier and better perception of Augmenter Reality projection compared to older generations. The study describes this ability build throughout the years of having the technology accessible in younger ages through games. As a result the augmented reality provides a lot of advantages compared to the other techniques and is considered to be better and very promising in the short-coming future [16].
Recently, it has been developed a system called Trans-Visible Navigation System, which allows surgeons to make use of Augmented Reality technologies and overlay into patient’s head intracranial structures. While the patient’s head is fixed in the operating table, a tablet pc is used for visualization purposes. Hence, the generated blood vessels or brain tumors are superimposed on the video image of the head, and allows correct angle projection while looking at the head from different positions (giving the feeling to the surgeon of seeing through the head) [17].
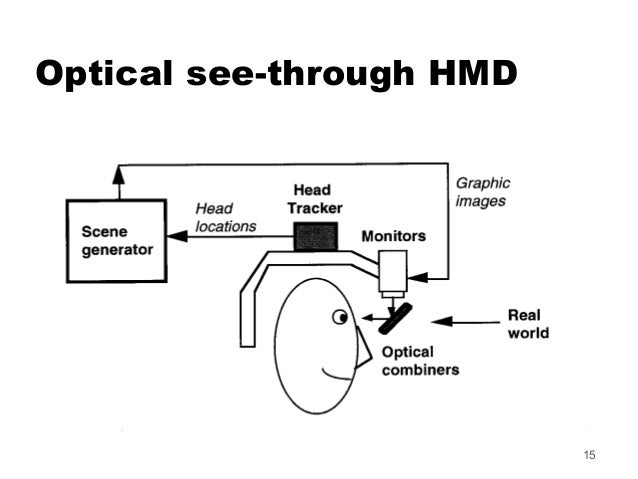
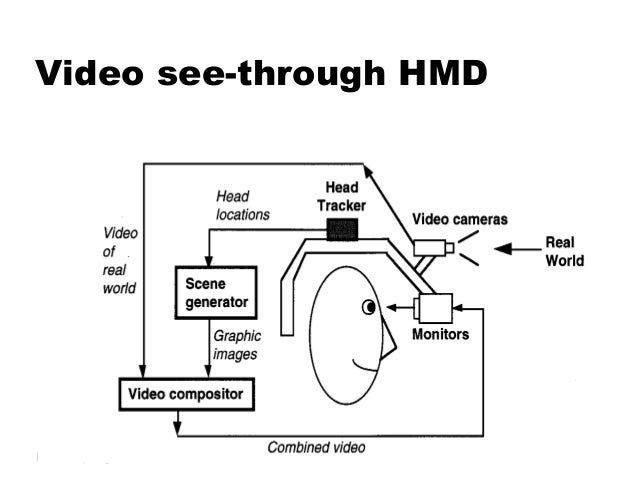
According to a research, there are many approaches on incorporating Augmented Reality into the surgery room. During the research, two methods have been depicted, a video see-through system and an optical see-through system. The optical see-through approach would not require the surgeon to have two video cameras head-mounted, would not require processing corresponding pair of video streams, and would provide a much higher resolution than is possible with current cameras. A video see-through approach composites the augmented view in a computer which allows much more control over the results. Basically, the difference between the two approaches is the source of information. In the video see-through approach, the surgeon has a head-mounted gear (cameras and display) which records the patient’s head and through two displays in-front of the eyes of the surgeon, gives the combined results (Augmented Reality information and video source) in the format of a video. In the optical see-through approach, the surgeon has a direct view in the patient and the optical gears only overlay augmented reality information on top of that [18].
Optical See-through HMD (left) and Video See-through HMD (right) [19][20]
Robotics
The human surgeon has a lot of advantages in respects to a robot, like its physical and mental flexibility to adjust itself to almost any situation or the ability to judge situations and decide based on the judgement. The most important part of the human body in comparison to a mechanical system is the highly developed hand-eye coordination that is difficult to reproduce with a robot. But problems like strength, stamina and accuracy are points where a robot is superior to the surgeon.
Therefore, the advances in robotics are complimentary to the advances in neurosurgery. The high accuracy, stamina and fast data processing of big data allow the surgeon to concentrate on the parts of a procedure where the above described advantages of a human surgeon are needed. Robots can and will be used to perform steady motions accurately or allow surgeons to operate remotely with a high reliability. Surgical robots can be classified in four different classes that are described in the next paragraph [21].
Classification
Classifying surgical robots considers the different degrees of autonomy of the robot and the degree of cooperation between the human and the machine [21]:
- Active systems are robots that perform parts of a neurological procedure completely autonomously and only is supervised by a surgeon. Such systems often have a high cooperation between robot and surgeon because the robot replaces interns.
- Semi-active systems perform procedures with guidance from the surgeon and help him in precisely positioning tools. The degree of cooperation is very high, since the robot corrects or helps the surgeons movements
- Passive systems provide the surgeon with information about the operation. Low degree of cooperation, because the robot serves as a navigational aid.
- Teleoperated systems are often master-slave systems that get orders from the surgeon (master) and the robot (slave) executes those exact orders
State of the Art
The first surgical robots where developed in the mid 80s based on industrial robots for the automotive industry. Since then the research has largely increased and surgical robots are a prominent of robotics research. In the following the newest robots are presented [22]:
- NeuRobot is a teleoperated robotic system developed in Japan that allows high precision procedures with minimal invasion. The surgeon can remove tumors or do other procedures by guiding the robot remotely. To navigate it only needs an opening of 10 mm.
- NeuroArm, developed in Canada, is like the NeuRobot an teleoperated robot that has better haptic feedback and allows for higher precision in surgery.
- EXPERT system is a passive robot that helps reduce fatigue in the surgeon.
- Steady-Hand-Systems try to decrease the effects of tremors in tumors hands during long surgeries [23].
NeuroArm setup before surgery [24]
Safety
In the above paragraphs, mostly advantages were presented, but in robotic neurosurgery the safety concerns are very high, since any mistake by the robot or the guiding surgeon can lead to severe brain damage or death. One main problem with robots and entire mechanical systems is the obligatory sterile environment in the operating room. It is very difficult sterilizing an entire mechanical system and is very expensive and needs to be repeated before every procedure. During the operation there is always the risk of a mechanical failure of the robot that leads to the surgeon having to finish the procedure without the robot. Such an situations requires the robot to be movable even if there is no power or the system is blocked at a precise location.
Ethical questions regarding the use of robots during surgery and especially in neurosurgery is part of a later discussion [21].
Future perspectives
Even if research in surgical robotics is very promising, progress is slow, because of the high cost of such research and the safety standards that have to be satisfied. The medical application of a research project needs to be safe to try on humans, which needs a lot of testing beforehand.
One focus of research lies in the integration of different imaging techniques into robot surgery and collect more data and be able to automate the surgical procedure more and relieve the surgeon some tasks. To minimize visual obstruction during an operation caused by a robot arm or the surgeon sophisticated camera systems are being developed that can help keep a certain visibility by adjusting the camera to the robot movement. A considerable problem concerning brain tumor surgery in general is brain shift due to the differences in CSF levels that make the brain shift in the skull. Actual research is trying to make it possible through medical imaging to detect movements of the brain and based on this data adjust the movements of the robot. To achieve this a high amount of data has to be processed in real time. This demands high power real time data transfers from a processing unit to the robot [22].
Another focus in research is teleoperated surgery and how to help the surgeon to get a better feedback from the robot. This is one over the haptic feedback the operator gets from the robot. Using new and more force measurement techniques, like visual force measurement and strain gauges, allows the robot to give the surgeon an exact feeling of how much pressure is being put on tissue.
Surgical robot with force feedback [25]
One direction of research tries to reduce the size of robots and tools to make them easier to integrate in an operating room and allow minimally invasive procedures to be performed by robots.
In the field of autonomous surgical robots, the development of new, more complex subroutines, like wound closing or clamping are being researched to make it possible for the surgeon to concentrate on the underlying surgical treatment.
A lot of this research can lead to future operations in which the surgeon is supported by four robot arms that take the place of interns and nurses and do tasks automatically or are controlled by another surgeon by tele guidance [23].
The near future can see stereotactic neurological procedures done by robots because of the superior accuracy of modern mechanical systems. Robotic stereo tactical radiosurgery can allow a high precision radiation of tumors delivered in a continuous motion. This makes it possible to destroy more cancerous tissue in the brain than actual human radiosurgery [26].
Stereotactic surgery [27]
References
- I. Mutchnick and T. M. Moriarty, “Intraoperative MRI in pediatric neurosurgery—an update,” Translational Pediatrics, vol. 3, no. 3, pp. 236–246, Aug. 2014.
- J. M. K. Mislow, A. J. Golby, and P. M. Black, “Origins of Intraoperative MRI,” Neurosurg Clin N Am, vol. 20, no. 2, pp. 137–146, Apr. 2009.
- http://tp.amegroups.com/article/viewFile/4164/5037/21810. [Accessed: 5-June-2017]
- http://photos.newswire.ca/images/20141029_C3516_PHOTO_EN_7227.jpg [Accessed: 5-June-2017]
- https://static1.squarespace.com/static/50305915e4b00d577d14e583/t/50933702e4b08a6452e932ed/1351825157935/IMIRIS-Room-Layout-Design-IntraOperative-MRI.jpg [Accessed: 5-June-2017]
- S. Zausinger, C. Schichor, E. Uhl, M. F. Reiser, and J.-C. Tonn, “Intraoperative CT in Neurosurgery,” in Intraoperative Imaging and Image-Guided Therapy, F. A. Jolesz, Ed. Springer New York, 2014, pp. 529–536.
- https://www.brainlab.com/en/surgery-products/overview-platform-products/intraoperative-ct/ [Accessed: 5-June-2017]
- G. Widhalm et al., “5-Aminolevulinic Acid Induced Fluorescence Is a Powerful Intraoperative Marker for Precise Histopathological Grading of Gliomas with Non-Significant Contrast-Enhancement,” PLoS One, vol. 8, no. 10, Oct. 2013.
- E. L. Rosenthal, J. M. Warram, K. I. Bland, and K. R. Zinn, “The Status of Contemporary Image-Guided Modalities in Oncologic Surgery,” Ann Surg, vol. 261, no. 1, pp. 46–55, Jan. 2015.
- J. T. C. Liu, D. Meza, and N. Sanai, “Trends in Fluorescence Image-guided Surgery for Gliomas,” Neurosurgery, vol. 75, no. 1, pp. 61–71, Jul. 2014.
- C. G. Janson, L. G. Romanova, K. D. Rudser, and S. J. Haines, “Improvement in clinical outcomes following optimal targeting of brain ventricular catheters with intraoperative imaging,” Journal of Neurosurgery, vol. 120, no. 3, pp. 684–696, Oct. 2013.
Augmented Reality Trends "Role of Augmented Reality in Medical Industry," Augmented Reality Trends, January 2014. [Online] Available: http://www.augmentedrealitytrends.com/augmented-reality/medical-augmented-reality.html [Accessed: 3-June-2017]
Christoph Bichlmeier, Felix Wimmer, Sandro Michael Heining and Nassir Navab "Contextual Anatomic Mimesis Hybrid In-Situ Visualization Method for Improving Multi-Sensory Depth Perception in Medical Augmented Reality," 6th IEEE and ACM International Symposium on Mixed and Augmented Reality, pp.129-138, November 2007.
Besharati Tabrizi L, et al., "Augmented reality-guided neurosurgery: accuracy and intraoperative application of an image projection technique," Journal of Neurosurgery, vol.123, no. 1, pp.206-211, July 2015.
IEEE, "Kinect + Brain Scans = Augmented Reality for Neurosurgeons," IEEE, video, March 2013. [Online] Available: https://www.youtube.com/watch?v=MvP4cHfUD5g [Accessed: 3-June-2017]
Springer - Augmented Reality Environments for Medical Imaging and Computer-Assisted Interventions. Lecture Notes in Computer Science, vol. 8090, pp. 241–248, Berlin, 2013.
Eiju Watanabe, et al., "The Trans-Visible Navigator: A See-Through Neuronavigation System Using Augmented Reality," World Neurosurgery, vol. 87, pp. 399-405, March 2016.
Calvin R. Maurer, et al., "Augmented reality visualization of brain structures with stereo and kinetic depth cues: System description and initial evaluation with head phantom," Medical Imaging 2001: Visualization, Display, and Image-Guided Procedures, pp. 445-456, February 2001.
Optical See-through HMD - Image [Online] Available: https://image.slidesharecdn.com/arppt-150422231121-conversion-gate01/95/augmented-reality-ppt-15-638.jpg?cb=1458653664 [Accessed: 3-June-2017]
Video See-through HMD - Image [Online] Available: https://image.slidesharecdn.com/arppt-150422231121-conversion-gate01/95/augmented-reality-ppt-16-638.jpg?cb=1458653664 [Accessed: 3-June-2017]
Zamorano L., Li Q., Jain S., Kaur G.: „Robotics in neurosurgery: state oft he art ad future technological challenges“ The International Journal of Medical Robotics & Computer Assisted Surgery DOI: 10.1581/mrcas.2004.01011
Mattei T., Rodriguez A., Sambhara D., Mendel E.: „Current state-of-the-art and future perspectives of robotic technology in neurosurgery“ Neurourgical Review DOI: 10.1007/s10143-014-0540-z
- Doulgeris J., Gonzalez-Blohm S., Filis A., Shea T., Aghayev K., Vrionis F.: “Robotics in Neurosurgery: Evolution, Current Challenges, and Compromises” Cancer Control July 2015, Vol.22 No. 3
- Optical See-through HMD - Image [Online] Available: http://www.neuroarm.org/wp-content/uploads/2010/04/project2.jpg [Accessed: 4-June-2017]
- TU Eindhoven, "Surgical robot with force feedback (Sofie)," TU Eindhoven, vidoe, April 2011. [Online] Available: https://www.youtube.com/watch?v=iIGy6K-vjpA [Accessed: 4-June-2017]
- Benabid A.L., Hoffmann D., Seigneueret E., Chabardes S.: „Robotics in neurosurgery: which tools for what?” in “Medical technologies in Neurosurgery” Springer Verlag
- TecnologieAvanzateTA, "ROSA 2011 Stereotactic Surgery," TecnologieAvanzateTA, vidoe, May 2013. [Online] Available: https://www.youtube.com/watch?v=6Jx2pc5XabM [Accessed: 4-June-2017]







Kommentar
Unbekannter Benutzer (ga48jeb) sagt:
06. Juni 2017Very well structured and layed out, made it easy to read. With lots of good information which is well sourced from the literature, good job!