| 10 Human Brain Fun Facts | |
|---|---|
1. The typical brain is about 2% of a body’s weight but uses 20% of its total energy and oxygen intake | |
| 2. Ninety minutes of sweating can temporarily shrink the brain as much as one year of aging | |
| 3. Your brain weighs about 3 pounds. Of that, the dry weight is 60% fat, making your brain the fattiest organ | |
| 4. No one knows for sure, but the latest estimate is that our brains contain roughly 86 billion brain cells. More than there are stars in in the Milky Way. | |
| 5. Each neuron connects with, on average, 40,000 synapses. | 6. Your right part of the brain directs the muscles in your left part of the body and vice versa. |
| 7. All brain cells are not alike. There are as many as 10,000 specific types of neurons in the brain. | 8. Only 5 minutes without oxygen can cause brain damage. |
| 9. Babies have big heads to hold rapidly growing brains. A 2-year-old’s brain is 80% of adult size. | 10. As any parent can attest, teen brains are not fully formed. It isn’t until about the age of 25 that the human brain reaches full maturity. |
Brain Anatomy
Central Nervous System (CNS)
The Central Nervous System, short CNS, consist of two main parts: the brain and spinal cord. The brain is surrounded and protected by the skull (see part of protection) and the spinal cord runs along the vertebral canal. In this article, we will concentrate on the brain, since the focus of this wiki lies on brain tumors.
Anatomy
The human brain has three main parts: the Cerebrum, the Cerebellum and the Brainstem. In the following we will take a closer look at each part.
- Cerebrum: has two cerebral hemispheres that are connected by corpus callosu; in every hemisphere, there are four lobes
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Cerebellum: lies posterior to the cerebrum, has many different compartments, that are connected to each other.
- Brainstem: lies under the cerebrum is the beginning of the spinal cord in the brain. Is connected to brain to allow muscle movement and control.
The typical surface of the brain has two major components:
- Suici are the brain folds on the surface
- Gyri are the smooth parts of the surface between the suici [1]
Illustration of the Cerebrum, Cerebellum and Brainstem [4]
Inner structure
Inner structure of the brain
There exist two main parts that define the inner structure of the brain: the outer part and the inner part.
The outer part, also called the cerebral cortex, consists of grey matter and contains a majority of nerve cell bundles.
The inner part, which lies inside the cerebral cortex, consists of white matter and mostly contains bundles of nerve fibers [1].
Location of white and grey matter [6].
Functions of the Brain
Every function, the brain is responsible for, is controlled by specific parts of the brain. In the following the different parts and their respective functions are listed:
The Medulla is responsible for basic bodily functions like the respiration, digestion and cardiovascular functions.
The Pons is also partly responsible for the right functioning of the respiration and it controls the inhibitions of the person.
The Cerebrum has two separated control tasks: the left hemisphere of the Cerebrum is controlling the right side of the body and the right hemisphere is tasked with the control of the left side of the body. The four lobes of the two hemispheres have specific control tasks:
- The frontal lobe is controlling speech, specialized motor controls, learning and planning
- The parietal lobe is in charge of the somatic sensory function
- The occipital lobe is controlling the vision
- The temporal lobe is tasked with the control of hearing and speech and contains the Hippocampus. This part of the temporal lobe is storing memories.
The Cerebellum uses the information from the eyes, joints, muscles and ears to compute the actual body position. The skeletal muscles are controlled by this part of the brain based on the new desired position, computed by the Cerebral CVortex. The Cerebral Cortex uses the somatic sensory information and calculates the new position. The Cerebellum is controlling the coordination, balance and posture of the human body and is used when learning a new motor function.
Furthermore, the Cerebellum is controlling parts of the emotions, but that is not its major task in the brain.
The Limbic System, that lies underneath the cerebrum, next to the thalamus and is controlling higher mental functions and primitive emotions.
The Amygdala is tasked with assuring the human self-preservation by controlling feelings, create fear and identifying dangers.
The Thalamus is in charge of emotional reactivity and the Hypothalamus is controlling vegetative functions, sexuality, hunger, combativeness and expressions of emotions.
The Cingulate gyrus is tasked with smelling, sights, memories of previous emotions, aggressivity and emotions to pain [3].
Location of the different brain functions.
Protection
To protect the brain from damage and ensure its proper function, the brain has developed different kinds of protection. First there is the anatomical protection that hast different layers. Most known protectors of the brain are the skin on your head and the skull bone, on which lies the skin and the hair. Under the skull there are 3 different membranes that are called meninges.
- Dura mater: tough membrane directly beneath the skull. It is found around the whole brain and the whole spinal cord.
- Arachnoid membrane: meninges located under the the dura mater
- Pia mater: vascularized membrane that is attached directly to the surface of the brain and of the spinal cord
To protect the brain from moving inside the skull, the space between arachnoid membrane and the pia mater is filled with a liquid, called the cerebrospinal fluid, short CSF.
Protecting the brain from dangerous molecules is the function of the blood-brain barrier [1].
Illustration of the meninges [5]
Cerebrospinal Fluid
Cerebrospinal Fluid
The cerebrospinal fluid, short CSF, is flowing in the cerebral ventricles, between the Arachnoid membrane and the Pia Mater. The cerebral ventricles are compartmented by the dura mater to ensure a constant level of CSF everywhere around the brain. The distribution of CSF fulfills two functions:
- restrict movements of the brain to cushion it and protect it against movements that can result in brain damage
- provide stable environment for proper neuronal function [1].
Blood-Brain Barrier
Blood-Brain-Barrier
The Brain is connected to the bloodstream to transport oxygen to the brain cells to guarantee the proper brain function. To assure that unwanted elements can’t harm the brain, the blood-brain barrier only let’s lipid-soluble molecules pass to the brain cells. Ionic solutes can’t pass the barrier. This mechanism allows to control the environment of the brain and by extension to protect the cells [1].
Neurons
There are many different types of neurons in the human body, but we will only treat the neurons that are found in the CNS. These neurons are called CNS neurons and are found in the grey matter of the brain. The cells develop branches, called dendrites, that connect nerve cells with each other and make it possible to exchange information between cells. To make the transfer of information possible, the cell body expands. This is called an axon.
This allows a nerve cell to connect to many different nerve cells and share information with those cells [1].
Schematic construction of a neuron [7].
Planes of the Brain
A standardized way to map the brain and in conclusion allow an easy and reliable method to map the brain. The mapping consists of partitioning the brain in slides, that are defined by planes and directions. There exist three planes: coronal, horizontal and transverse. The five directions give the exact orientation of the slice: rostral, superior, ventral, caudal, dorsal [2].
The different planes and orientations describing the brain [8].
Brain Tumor Symptoms
The causes of brain tumors are not well known, but there exist some things that are known to increase the risk of being diagnosed with a brain tumor. For example, a high dosage of X-ray radiation on the head, is elevating the risk of getting a brain tumor.
The most common symptoms are chronic headaches, seizures, vomiting, nausea, numbness in some body parts. These symptoms often don’t occur all at once, but separately, because a tumor is pressing on the specific part of the brain that controls this function [3].
Brain Tumor Diagnosis
There are several techniques when it comes to brain tumor diagnosis. These techniques vary from invasive (early methods of tumor identification) up to more advanced through powerful imaging modalities. These different techniques are used in order to identify the location of the tumor, weather it started in the brain or it has metastasized from another part of the body, or even if it has spread from the brain towards the body (according to Cancer.net it is very rare). The straightforward way of diagnosis is by doing a biopsy, which samples are analysed in laboratory and an exact diagnosis is give. However, this method is very invasive and sometimes even not possible. But before going to biopsy, doctors suggest performing some imaging techniques, which give insights from the body and decide the presence of a tumor or not [9].
Most commonly the brain tumors are diagnosed after some symptoms are witnessed by the patient. An Internist or Neurologist would firstly recommend an MRI as an initial diagnosis. In case the presence of a tumor in the brain is confirmed, there are further techniques used in order to determine the type of tumor, grading and preparation for treatment. All the different techniques in order to diagnose brain tumors are explained in more detail in the following paragraphs [9].
Neurological Examinations
A neurological examination is usually conducted in the first steps of determining the presence of a tumor or not. Usually the physician checks the vision, balance, hearing, muscle strengths, coordination and reflexes. Any difficulties in one or more areas mentioned before, provides enough grounds for further examinations in order to determine the presence of the tumor in the brain. Furthermore, these tests may include checking the eye in more detail for any swellings coming from the pressure to the vision nerves between the eye itself and the brain [10][11].
Imaging Techniques
Depending on the results from the above test, physicians may request the patient further analysis through imaging techniques. These techniques give more insights from the patient's brain, where they are able to determine the presence of a tumor. Some of these techniques are discussed in the paragraphs below.
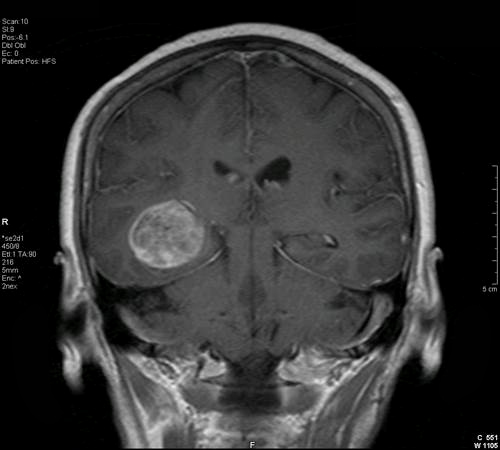
Magnetic Resonance Imaging (MRI)
One of the commonly used imaging techniques for brain tumor identification is the MRI technique. MRI uses magnetic fields to produce images of the body, which in brain tumor cases, forms detailed images of the brain. Very powerful magnetic fields surround the head of the patient, and in alternation with radio waves produce very detailed brain images. These images are produced as slices and can be further combined to create a 3D model of the brain, more particularly, potential tumors in the brain. Nevertheless, in some cases the MRI is performed after a dye (contrast medium) is injected in the patient's arm, this helps the images to be more detailed and clear [9][10][12].
Brain Tumor (MRI), Transversal view (left), and Coronal view (right) [13][14].
Computed Tomography (CT)
Computed Tomography is one of the imaging techniques used for tumor identification as well. Similar to a MRI, a CT can take detailed images of the brain, however it uses x-rays in order to produce the images. A contrast agent is usually injected which makes the abnormal tissues and areas of the brain easier to see [10]. These type of images are very good at identifying brain tumors near the skull, or even tumors which involve the bone of the skull. Furthermore, CT scans can show very clearly any swelling, bleeding and bone - tissue classification [12].
Positron Emission Tomography (PET)
Positron Emission Tomography is one of the techniques used in order to have more details about the tumor, or even in cases when there is a tumor relapse (recurrence). This procedure usually is combined with a CT, but it is referred as a PET only. Before the scan, a radioactive glucose substance is injected to the patient, due to the high consumption of energy by the tumor cells, there can be identified a concentration of the radioactive substance through the PET images [9][12].
Brain Tumor (PET Imaging) [15]
Cerebral Arteriogram (Angiogram)
Cerebral Arteriogram or also known as Angiogram, is an x-ray image, or multiple x-ray images of the head. Before the images are taken, a contrast agent is injected to the patient in order to make the main arteries of the brain visible. In case a tumor is present, through this imaging technique the physician is able to locate the tumor and identify the vessels feeding the tumor [9][10].
Cerebral Arteriogram, Sagittal view (left), Coronal and Sagittal view (right) [16][17]
Functional MRI (fMRI)
Functional MRI is a special techniques used for brain tumor identification. Although not directly involved in brain tumors, fMRI is a technique that identifies activities in the brain. Different activities of the human body, such as movement, speaking etc, produce different MRI images at a very slight signal change, these changes are depicted from the fMRI and pinpoint activity centers in the brain. Through these images, physicians are able to identify vital activities and their location in the brain, in order to be careful and do detailed planning for surgery. An example is when the brain tumor is located very near the part of the brain in charge for movement of muscles (legs and arms), during planning of the surgery, physicians are informed for which parts of the brain to be more careful and avoid [12].
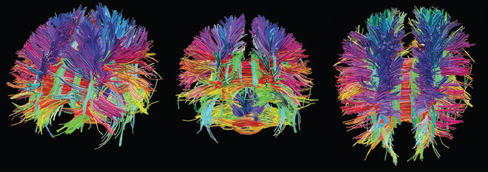
Diffusion Tensor Imaging (DTI)
Similar to fMRI, Diffusion Tensor Imaging is not a technique used directly for brain tumor identification, but it is used for planning and surgery. DTI measures and visualizes the flow of water (circuitry of the brain) through the white matter or the brain [12].
Diffusion Tensor Imaging [18].
Magnetic Resonance Spectroscopy (MRS)
Magnetic Resonance Spectorcopy is one of the other non-invasive imaging techniques used for identification of chemical abnormalities in the brain. This techniques is used for identification of infecitons, strokes, Alzheimer's disease, Multiple Sclerosis and tumors. MRS is captured similarly as MRI, however the difference is that MRS captures the function of the brain, similar to fMRI, compared to MRI which captures the structure of the brain. The main advantage of the MRS is that it can capture some features of the brain which are important for tumor identification that cannot be captured by the MRI [12].
Magnetic Resonance Spectroscopy [19]
Myelogram
This method is rarely used, however it is very important to identify if the tumor has spread to the Cerebrospinal Fluids, spinal cord or other parts of the brain. It uses a dye injection in the brain, which shows very well in an x-ray and help the doctors look for a tumor [9].
Invasive, noninvasive and other lab test
Spinal Tap
Spinal Tap or also known as Lumbar puncture, is an invasive procedure where a needle is used to take samples from the cerebrospinal fluid to analyse the tumor cells, blood, and tumor markers. Tumor markers or biomarkers are substances in the body which are in higher levels in case of the presence of a tumor. This procedure is preformed with local anesthesia in the proximity where the needle punctures the body. The procedure is relatively short, around 30 minutes, however the patient has to lie flat for several hours to avoid headache [9][10].
Spinal Tap procedure [20]
Evoked potentials
Through this test, physicians are able to identify electrical activity of nerves and can very often detect noncancerous brain tumor (acoustic schwannoma). This method makes use of electrodes which are connected to the patient and are used best as a guide when removing a tumor near important nerves of the body [9].
Neurocognitive Assessment
Neurocognitive assessment consists of very detailed test in regards to the main functions of the brain, such as memory, expressiveness, logical problems, calculations and overall well being of the patient. Upon completion, a report is issued and used for further comparisons, which would help to identify lacking problems and adopt the treatment [9].
Electroencephalography (EEG)
This is a non-invasive test, similar to evoked potentials, used to identify electrical activity of the brain. It can be used for monitoring and identification of possible seizures. EEG provides continuous measures of cerebral functions over time, which functionality cannot be provided by other imaging techniques mentioned before [9][21].
Biomarkers
Biomarkers stands for Biological Marker which associates with Indicator. These biomarkers are captured and represent a change in the genes of the tumor's DNA, or it can be a molecule produced by the tumor. A biomarker test may be used to look at genes associated with the type of tumor [22]. The test are helpful for
- Identifying the type of tumor
- Growth prediction
- Predicting treatment response
- Planning treatment
Tumor Types
Tumors are classified based on their tissue of origin. Any tumor that originates in the brain is called primary brain tumor. A tumor that comes from another tissue and has metastases in the brain is a secondary brain tumor. A distinction is made between benign tumors and malignant ones. The first category is in locally confined and does not spread in surrounding tissues. Malignant or cancerous tumors express this characteristic and are therefore intrinsically dangerous for the organism. Allthough not primarily lethal, benign tumors may have negative effects on health, since the growing tissue may inflict pressure on sourrounding areas or organs, which is especially severe in the case of brain tumors, because the cranial space is limited. Furthermore any benign tumor has the capacity to develop into a cancerous one, a process known as tumor progression [23][24][25].
Nomenclature
Generally, tumors are classified by the cell they originate from and its behaviours. The following nomenclature for tumors has been introduced with the new WHO classification system of 2016 [26]. A diagnosis consists of the histopathological name (e.g Diffuse astrocytoma), followed by (multiple) genetic features (e.g IDH-mutant or IDH-wildtype, if available, or NOS if a genetic diagnosis is not possible). The revised scheme comprises 17 superclasses, each having a varying amount of subclasses and has major differences to the previously used system of 2007 [27]. The traditional diagnosis scheme using histology is now complemented by genotyping, favored by the increasing availability of sequencing technologies in the post-genomic area. One expected result is an improved objectivity and reproducibility of the diagnosis helped by the analysis of the individual genetic material of the tumor. The classes are more narrowly defined, and include mutation status of genes which have been found to be altered in many tumors, such as IDH in gliomas [28]. In the following a brief non-exhaustive characterization of the different tumor classes will be presented.
Table 1: The tumor classes according to the new classification scheme of 2016 [26].
Gliomas
The most commonly observed tumor type in adults are gliomas, which originate from glial tissue, mainly in the brain but may also arise in other parts of the CNS. Most gliomas behave in a malignant fashion and cause significant mortality in adult brain cancer patients. Diffuse astrocytic and oligodendroglial tumors represent the largest subgroup of gliomas, comprising glioblastoma, astrocytoma, oligodendroglioma and oligoastrocytoma with variing grades (also see table 2 ). The overall survival prognosis is very poor, with only 0.5-4.7% of the patients alive 5 years after the diagnosis. The median survival period is 15 month. An oligodendroglial component seems to increase the survival probability in comparison to to astrocytic gliomas. The age of onset largely depends on the tumor type. Anaplasic astrocytomas and gliobastoma occur on average later in life (75-84 years), while oligodendrogliomas and oligoastrocytomas more commonly appear between the age of 35 and 44. Other than age, gender and race seem to have an influence on the susceptibility to different types of tumours, however many studies remain inconclusive. In recent years, a number of biomarkers have been established, which help the catergorization of the different subtypes and give insight in the disease pathologies such as altered gene expression (e.g of EGFR) and DNA methylation. Genome-wide assosication studies (GWASs) favor a multigenic inheritance pattern for glioma risk since several SNVs have been associated with different tumor types, but no major driving allele could be identified to date. Allergies are correlated with an decreased brain tumour risk. Cell phone use, can for instance not be linked to an increased brain tumor risk, however delayed effects can not be investigated at the moment, since the massive use of mobile devices is a rather young phenomenon [31][32][33].
Figure: The relative frequency of histopathologically diagnosed oligodendroglial and oligoastrocytic tumors in the spectrum of glial tumors if the CNS a) in 95,564 patients of all age groups; b) in 10,274 children and adolescents (0-19 years); Figure taken from [34].
Tumor Grading
Generally tumors are graded according to the standard grading scheme spanning four classes:
- Grade 1: the cells look almost normal in terms of tissue appearance and organization – they are well differentiated. Tumors of grade 1 have a low proliferative potential, are non-invasive and may be cured via surgery.
- Grade 2: The tumor exhibit abnormal cells (moderately differentiated) and are invasive, but show low proliferative activity. However they may transform to higher grade tumors and recur more often.
- Grade 3: The cells in those tumors look abnormal (undifferentiated) and proliferate quickly such that the tumor spreads. A tumor is of grade 3 if evidence of malignancy can be observed. Grade 3 tumors are generally treated using radio- or chemotherapy.
- Grade 4: The cells in the tumor are actively dividing in an undifferentiated manner and spread in the surrounding tissue can be observed. Those tumors mostly have fatal outcome [29][30].
In 2016, with the update of the classifiction scheme for brain tumors, the grading has begun to include genetic features such as mutations in specific genes and stopped relying on histological features alone. The table below shows an excerpt of the WHO tumor grading guideline from 2016.
Table 2: Selected tumor grades of the new brain tumor classfication scheme [26].
The grade of a tumor is one component of the overall prognosis for the patient. Other factors are for example age and location of the tumor, as well as available treatment options.
Lymphomas
Lymphomas are the second most common malignancy of the central nervous system and account for approximatly 3-5% of the brain tumors. They do not only arise in the brain, but also in the eyes, leptomeninges and spinal chord. The most abundant class are diffuse large B-cell lmyphomas, a minority are T-cell- and low-grade B-cell lymphomas. The Eppstein-Barr virus is linked to the outbreak of lymphomas in immunocompromised patients, but causes of the tumors in immunocompetent patients are scarcely elucidated to date. A lower incidence has been observed in people suffering from AIDS. The prognosis is generally poor with many recurrences, although the prognosis has improved in the last years. Surgery is used only for diagnostic purposes, the current treatment option is methotrexat-based chemotherapy in combination with radiotherapy [35][36][37].
Embryonal tumors
Brain tumors are the third most common tumor types in children and in most cases malignant. About 20% of the pedriatic brain tumors are of the embryonal type. They spread via the cerebrospinal fluid to other parts of the brain, to the spinal chord and rarely to other parts of the body. Medulloblastoma account for most of the juvenile brain malignacies. It is believed, that they arise from embryonic stem or precursor cells which remain in the brain after birth and are poorly differentiated. They most often arise between the age of 1 and 9, the median age of onset is 6. Boys are have an about 1.5 fold higher risk of having a brain cancer and usually have a worse prognosis than girls. Other embryonic tumor types are primitive neuroectodermal tumors [PNETs], medulloepithelioma, and atypical teratoid/rhabdoid tumors [AT/RTs] [38][39][40].
Other tumor types
- Chroroid plexus tumors
- Neuronal and mixed neuronal-glial tumors
- Tumors of the pineal region
- Tumors of the cranial and paraspinal nerves
- Meningiomas
- Mesenchymal, non-meningothelial tumors
- Melanocytic tumors
- Histiocytic tumors
- Germ cell tumors
- Tumors of the sellar region
- Metastatic tumors
References
- Pocock, Gilian; Richards, Christopher D. “Human Physiology: The Basis of Medicine” Oxford Core Texts. ISBN: 978-0198568780
Waxman, Stephen G. “Clinical Neuroanatomy” McGrawHill- Education. ISBN: 978-1259095313
- Roger, Kara. “The Human Body: The Brain and The Nervous System” Britannica Educational Publishing. ISBN: 978-1615301362
Brain map. [Online] Available: http://humanbrainfacts.org/images/resource/human-brain-mapping.jpg. [Accessed: 9-May-2017]
- Meninges. [Online] Available: http://4.bp.blogspot.com/-C_SMaJ24IMY/UOvRZh-sKmI/AAAAAAAAAVg/OJElASyDDVY/s1600/meninges+2.jpg. [Accessed: 9-May-2017]
- Inner structure. [Online] Available: http://www.medinewsdigest.com/wp-content/uploads/2011/12/Brain_Cortex_Harvard.png. [Accessed: 9-May-2017]
- Neuron. [Online] Available: https://online.science.psu.edu/sites/default/files/bisc004/content/neuron.jpg. [Accessed: 9-May-2017]
- Planes of the brain. [Online] Available: http://homepage.smc.edu/russell_richard/Psych2/Graphics/Brain_directions_planes__sections_1_small.gif. [Accessed: 9-May-2017]
- Cancer.net, "Brain Tumor: Diagnosis," Cancer.net, June 2016. [Online] Available: http://www.cancer.net/cancer-types/brain-tumor/diagnosis. [Accessed: 9-May-2017]
- Brain Cancer Breakthroughs, "Diagnosis," abc2.org [Online] Available: http://abc2.org/guidance/brain-cancer-facts/diagnosis. [Accessed: 9-May-2017]
- Mayo Clinic, "Brain Tumor Diagnosis," Mayo Clinic, January 2016. [Online] Available: http://www.mayoclinic.org/diseases-conditions/brain-tumor/diagnosis-treatment/diagnosis/dxc-20117172 [Accessed: 9-May-2017]
- Johns Hopkins Medicine, "How to Diagnose Brain Tumors," Johns Hopkins. [Online] Available: http://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/brain_tumor/diagnosis/how-to-diagnose-brain-tumors.html [Accessed: 9-May-2017]
- MRI Image 1. [Online] Avaialble: https://images.radiopaedia.org/images/5651/b510dc0d5cd3906018c4dd49b98643.jpg. [Accessed: 9-May-2017]
- MRI Image 2. [Online] Avaialble: http://www.neuralregeneration.org/images/Brain_Tumor_Coronal.jpg. [Accessed: 9-May-2017]
- PET Image. [Online] Avaialble: http://jnm.snmjournals.org/content/52/6/865/F1.large.jpg. [Accessed: 9-May-2017]
- Angiogram Image 1. [Online] Avaialble: http://www.rctradiology.com/icons/Normla~1.jpg. [Accessed: 9-May-2017]
- Angiogram Image 2. [Online] Avaialble: http://texasradiology.com/wp-content/uploads/2013/10/cerebral-angiography.png. [Accessed: 9-May-2017]
- DTI Image. [Online] Available: https://www.nap.edu/openbook/13373/xhtml/images/p26.jpg. [Accessed: 9-May-2017]
- MRS Image. [Online] Available: https://media1.britannica.com/eb-media/57/183157-004-47ACA1A5.jpg. [Accessed: 9-May-2017]
- Spinaltap Image. [Online] Available: https://medical.azureedge.net/images/lumbar-puncture-diagram1.png. [Accessed: 9-May-2017]
- David Y Ko, "EEG in Brain Tumors," Medspace, March 2014. [Online] Available: http://emedicine.medscape.com/article/1137982-overview. [Accessed: 9-May-2017]
- The Brain Tumor Charity "Biomarkers," thebraintumorcharity, March 2014. [Online] Available: https://www.thebraintumourcharity.org/understanding-brain-tumours/getting-a-diagnosis/biomarkers/. [Accessed: 9-May-2017]
- “Understanding Brain Tumors.” [Online]. Available: http://braintumor.org/brain-tumor-information/understanding-brain-tumors/. [Accessed: 03-May-2017].
- “Benign tumor,Wikipedia. 15-Mar-2017.
- “Tumor Types - National Brain Tumor Society.” [Online]. Available: http://braintumor.org/brain-tumor-information/understanding-brain-tumors/tumor-types/. [Accessed: 30-Apr-2017].
- D. N. Louis et al., “The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary,” Acta Neuropathologica, vol. 131, no. 6, pp. 803–820, Jun. 2016.
- D. N. Louis et al., “The 2007 WHO Classification of Tumours of the Central Nervous System,” Acta Neuropathologica, vol. 114, no. 2, pp. 97–109, Jul. 2007.
- A. Cohen, S. Holmen, and H. Colman, “IDH1 and IDH2 Mutations in Gliomas,” Curr Neurol Neurosci Rep, vol. 13, no. 5, p. 345, May 2013.
- “Tumor Grade Fact Sheet - National Cancer Institute.” [Online]. Available: https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis/tumor-grade-fact-sheet. [Accessed: 07-May-2017].
- “Brain Tumor: Grades and Prognostic Factors | Cancer.Net.” [Online]. Available: http://www.cancer.net/cancer-types/brain-tumor/grades-and-prognostic-factors. [Accessed: 07-May-2017].
Q. T. Ostrom et al., “The epidemiology of glioma in adults: a ‘state of the science’ review,” Neuro-Oncology, vol. 16, no. 7, pp. 896–913, Jul. 2014.
J. Bianco, C. Bastiancich, A. Jankovski, A. des Rieux, V. Préat, and F. Danhier, “On glioblastoma and the search for a cure: where do we stand?,” Cellular and Molecular Life Sciences, Feb. 2017.
- J. P. Thakkar et al., “Epidemiologic and Molecular Prognostic Review of Glioblastoma,” Cancer Epidemiology Biomarkers & Prevention, vol. 23, no. 10, pp. 1985–1996, Oct. 2014.
P. Wesseling, M. van den Bent, and A. Perry, “Oligodendroglioma: pathology, molecular mechanisms and markers,” Acta Neuropathol, vol. 129, no. 6, pp. 809–827, 2015.
D. Ricard, A. Idbaih, F. Ducray, M. Lahutte, K. Hoang-Xuan, and J.-Y. Delattre, “Primary brain tumours in adults,” The Lancet, vol. 379, no. 9830, pp. 1984–1996, 2012.
- J. Yun and F. M. Iwamoto, “Primary Central Nervous System Lymphoma: A Critical Review of the Role of Surgery for Resection,” Archives in Cancer Research, vol. 4, no. 2, 2016.
K. Hoang-Xuan et al., “Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: guidelines from the European Association for Neuro-Oncology,” The Lancet Oncology, vol. 16, no. 7, pp. e322–e332, 2015.
M. Tulla et al., “Incidence, Trends, and Survival of Children With Embryonal Tumors,” PEDIATRICS, vol. 136, no. 3, pp. e623–e632, Sep. 2015.
N. L. Drezner and R. J. Packer, “The impact of molecular analysis on the survival of children with embryonal tumors,” Translational pediatrics, vol. 5, no. 1, p. 5, 2016.
- “Childhood Central Nervous System Embryonal Tumors Treatment (PDQ®)—Patient Version - National Cancer Institute.” [Online]. Available: https://www.cancer.gov/types/brain/patient/child-cns-embryonal-treatment-pdq. [Accessed: 08-May-2017].















2 Kommentare
Unbekannter Benutzer (ga38gis) sagt:
13. Mai 2017Your wiki is pretty detailed - I like that!
My ideas for improvement are listed below. Of course everything is just a suggestion :).
I would prefer more citations directly in the text, so I don't have to look for it if I want to see your source (but that's only my opinion). Additionally, when I see the source [abc2], it is not that easy to find to which source it belongs. Also links to the source would be nice.
I found some spelling errors and marked them directly in the text (e.g. symptom
Es).Your list of contents contains a dot without text (the first one). I think that's by mistake?
You're not completely consistent in whether you write technical terms capitalized or not (section Functions of the Brain: thalamus vs. Hypothalamus). The same for image descriptions (in section Inner structure capitalized, in section Planes of the Brain not capitalized).
I know I am pretty picky, but your wiki is nice! These are just some little things I recognized while reading your article ;).
Ardit Ramadani sagt:
14. Mai 2017Thanks for the feedback!
The work presented until now is not the final version which we have in mind. Regarding the references you mentioned, the problem is that we have worked separately and in the following meeting we will finalize the numbering, consistency of appearance, and also the linking (I know it is hard to find where in the bibliography is a specific reference located. But when we finalize the numbering and other details in the references we will link them in order to redirect at the specific location at the end of the wiki).
As for the spelling errors and grammatical mistakes, we have read through it and one of the team members has already fixed some of the mistakes.
I hope you enjoy and find the wiki helpful!