Radiation therapy can be used to locally target tumors that are not spread over the whole body. Therefore the patient is exposed to e.g. photon radiation (x-rays) in order to damage the tumor cells.
Radiation effects
Primary target for the radiation is the DNA of the tumor (in cell nucleus). If the DNA is too damaged, the cell dies within hours (apoptosis). If the cell survives with some damage or mutations and it can't be completely repaired, the tumor cells might still die after a few cell cycles (reproductive cell death).
For choosing the dose of radiation a balance must be found between tumor control and side effects. Fortunately tumor cells usually show a higher biological effect than healthy tissue when being exposed with the same dose. Even then, high-dose radiation can pose an additional risk as e.g. new tumors can evolve due to the DNA damage of healthy cells. [1][2][3]
Fractionation
Nowadays usually the radiation dose is divided into smaller radiation portions over time to decrease the radiation effect on normal tissue. This procedure is called fractionation. The approach is based on the fact that usually healthy cells have a better DNA repair mechanism than tumor cells. To give the cells enough time for repairs, the irradiation doses must be sufficient time apart. Typical values are for example: dose of 60 Gy divided in 30 fractions of 2 Gy, distributed over 40 days. [2][4]
Radiation types
Radiation types for radiation therapy are:
- Photons
- Electrons
- Pions (π -)
- Protons
- Neutrons
- Ions
These days in general only photons (x-rays), electrons, protons and ions like 4He2+ or 12C6+ are used. [2]
Proton beam therapy
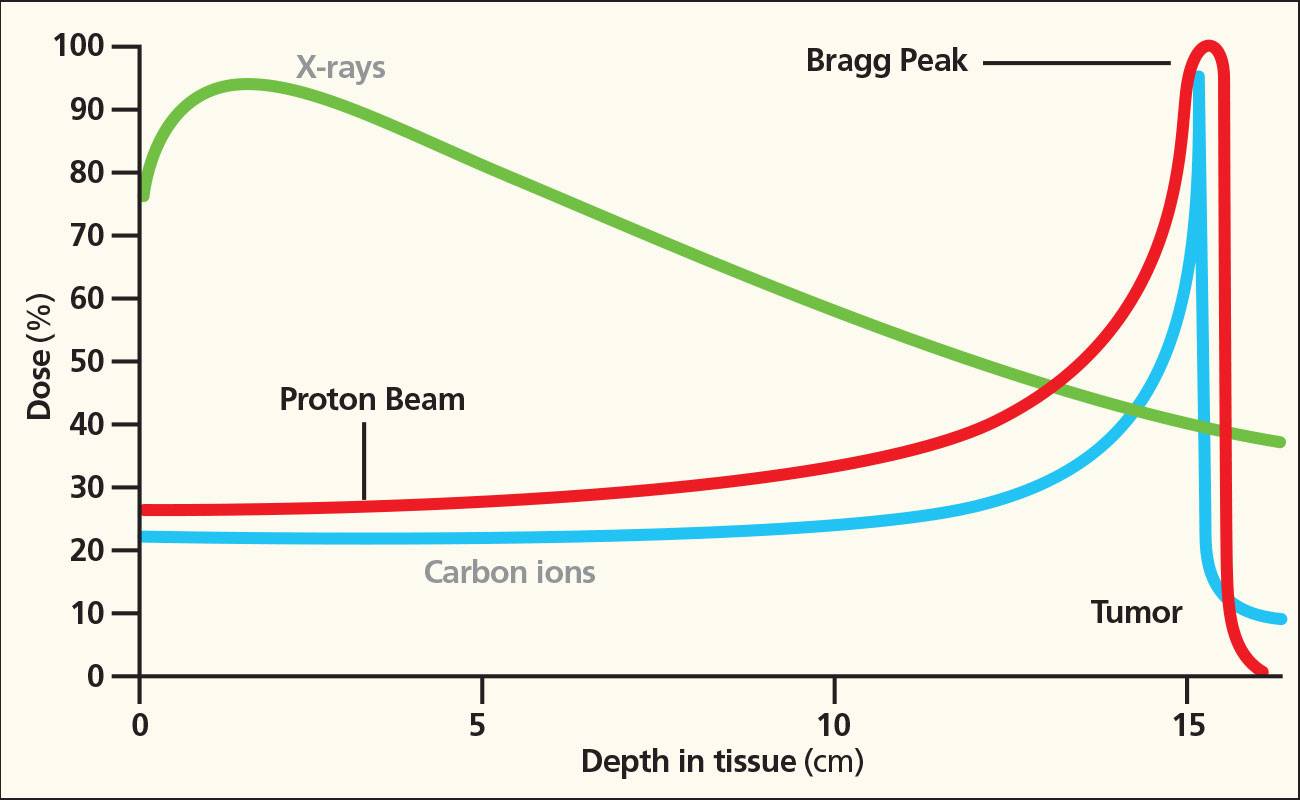
Protons as a radiation type are interesting because of their dose distribution over depth in the tissue.
figure: Dose over depth in tissue. Proton and ion beam vs. x-rays. [5]
Unlike photons (x-rays), the maximum dose of protons is deeper in the tissue, immediately before the particles come to rest. Hence they are ideal for the irradiation of tumors as on the way through the surrounding tissue the dose is lower, at the target the dose is maximal and in the area behind the tumor the dose is almost zero. The peak is called the Bragg peak. This is extremely beneficial if the tumor is adjacent to areas of the brain that control vital functions.
This applies also for ion beams such as 4He2+, 12C6+, etc. (see figure above). [6]
Radiation therapy treatment
External beam radiation is the most common form of radiation therapy for brain tumors. [7] For planning the treatment, usually several brain scans are made to determine the exact location and shape of the tumor.
To achieve precise targeting of the tumor, often several beams from different angles are superposed. Hence the radiation dose for the surrounding tissue is lower.
figure: Beam superposition. [7]
Radiotherapy is called stereotactic radiation therapy, if scanners (CT, MRI, ..) are used to very accurately locate the tumor. Additionally the position of the head of the patient is strictly held in place during the treatment. Thus the tumor is irradiated with a sufficiently high dose while the healthy tissue is precisely spared. Due to the accuracy of the superposed beams it is possible to do the treatment in only one session (stereotactic radiosurgery). Stereotactic radiotherapy or -surgery are used for small brain tumors (≤ 3 cm).
To prevent brain swelling often steroids are given before the treatment. [8]
Side effects
Radiotherapy does not only destroy the tumor cells but also harms the surrounding healthy tissue. Furthermore radiotherapy can cause swelling of the tissue and thus additional pressure on the brain.
Short-term side effects
- Fatigue
- Headache
- Feeling sick, dizzy or faint
- Hair loss
- Seizure
Long-term side effects
- Radiation necrosis (6-24 months after treatment)
- Rarely new tumors evolve due to the DNA damage of healthy cells [8]
Bibliography
1) Krieger H. (2007) Grundlagen der Strahlungsphysik und des Strahlenschutzes, 2. Auflage, Teubner: Wiesbaden
2) Hall E. J. (2000) Radiobiology for the Radiologist, Lippincott: Philadelphia, 5th ed.
3) Steel G. G. (2002) Basic Clinical Radiobiology, Arnold: London, 3rd ed.
4) Joiner M. (2009) Basic Clinical Radiobiology, Arnold: London, 4th ed., https://phyusdb.files.wordpress.com/2013/03/basic-clinical-radiobiology.pdf
5) hi_res_bragg_peak.jpg, https://www.scripps.org/sparkle-assets/images/hi_res_bragg_peak.jpg (access 29/05/17)
6) Paganetti (2002) Physical Medical Biology
7) Radiation Therapy, http://www.abta.org/brain-tumor-treatment/treatments/radiation-therapy.html (access 29/05/17)
8) Figure-1-A-schematic-of-a-multi-beam-radiation-treatment-plan-for-a-brain-tumor-is.png, https://www.researchgate.net/profile/Adam_Glaser/publication/264983469/figure/fig1/AS:295985499656192@1447579850070/Figure-1-A-schematic-of-a-multi-beam-radiation-treatment-plan-for-a-brain-tumor-is.png (access 29/05/17)
9) Stereotactic radiotherapy, https://www.thebraintumourcharity.org/understanding-brain-tumours/treating-brain-tumours/adult-treatments/stereotactic-radiotherapy/ (access 29/05/17)