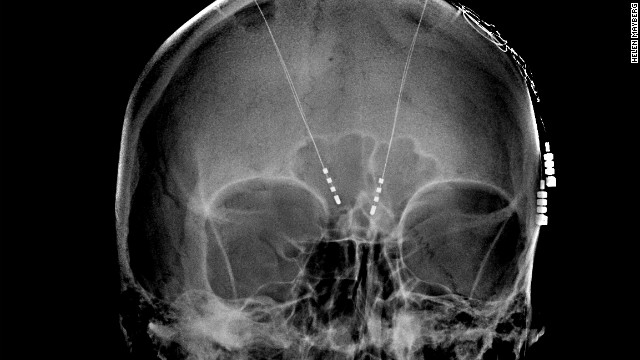
Frame vs Frameless
There are some proponents of frame-based approaches which claim that although both frame and non-frame based techniques are equally effective for use (here, in intracranial biopsies) the frame-based approaches were shown to require fewer anaesthesia resources and produce shorter OR times (by approximately an hour) and hospital stays for the patient (Smith, et al., 2005). Contrastingly, proponents of frameless approaches make similar claims about their technique – specifically in shorter OR, and anaesthesia times as well as shorter hospital stays (Dorward, et al., 2002). In addition, Dorward, et al. (2002) finds that the complication rate for frameless biopsies is less than for framed biopsies.
Advantages & Disadvantages
There are other advantages to frameless approaches (Lobão, et al., 2009):
- More comfort to the patient due to the lack of stereotactic frame
- Same levels of complications and diagnostic efficiency as framed approaches (see also Dammers, et al. (2008))
- The surgical instruments used in frameless approaches occupy less space than those used with the frame
- The trajectory of the biopsy needle can be changed at any time during the surgery without new calculations being needed
There are of course disadvantages too (Lobão, et al., 2009):
- Precision is closely related to the pre-operative imaging
- Requires accurate registration, depending on the method used for the registration navigational accuracy can be reduced
- Is usually done using general anaesthesia which carries higher risks to the patient than framed methods which use sedation and local anaesthesia.
- The use of general anaesthesia reduces the ability for the doctors to perform a neurological evaluation immediately after the procedure.
- The costs of acquiring a frameless system are high, which can be a barrier to their use, particularly in emerging countries. Note though that the long-term cost (accounting for reduced complications etc.) is lower.
Bjartmarz & Rehncrona suggest a number of reasons for this outcome have been suggested. First, in the frame-based approach the brain is registered from the beginning in relation to a skull-fixed frame using a computer planning system with six different MRI indicators; whereas in the frameless system has fewer markers for registration. Additionally, the position of the markers has to be verified by hand by the surgeon. It is though that the increased number of interfaces and information transfers may make the frameless approach more susceptible to error.
Second, in the frame-based approach the surgical target is always located in the center of a sphere and the trajectory is a radius with its movement axis in that location. Contrastingly, the frameless approach has its movement axis close to and above the skull bone to facilitate better movement in the surgical target area. This means that if there is any instability in the frameless system then the small angular variations this would cause can have a large effect on the final location of the electrode.
Interestingly, despite the differences in electrode placement the clinical outcome was the same with both techniques – that is the tremor reduction was similar for both framed and frameless techniques. Although this means that either approach can be used for this treatment Bjartmarz & Rehncrona note that this does not necessarily hold true for other surgical procedures where there are smaller targets, requiring higher accuracy to achieve a clinical effect.
Other Factors Affecting Accuracy
Registration Method
Frameless stereotaxy requires a registration to be made between the pre-operative and interoperative images. One of the main ways this is done is using fiducial markers and a point-pair registration but anatomical landmarks can also be used as can surface matching. Each of these registration approaches has a different accuracy. This accuracy is given as the target registration error or TRE which is the Euclidean distance between the image space coordinates and world space coordinates of a target marker. The target marker is separate from the registration markers and is used to simulate a surgical target.
A study by Woerdeman, et al., (2007) found that regardless of the target location or imaging modality adhesive markers were the most accurate way of performing a registration with mean accuracy of 2.49mm compared to 5.03mm for surface matching and 4.97mm for the use of anatomical landmarks.
Of course, fiducial markers can only be used for planned registration where the patient has the markers placed before being sent for imaging. If images from earlier studies are used then anatomical landmarks and surface mapping can be used.
Registration Sequence
It has been found that when scalp fiducial markers are used for registration there is no impact on accuracy of the order in which the markers are registered (Smith, et al., 2014).
Marker Arrangement
Fiducial arrangements distributed optimally across the skull, however, allowed for significantly improved accuracy.
When using fiducial markers a number of errors can occur (Smith, et al., 2014):
- Fiducial localization error – the difference between where a fiducial is in the image space and where it is in the patient space, e.g. due to movement of the markers between imaging and surgery.
- Fiducial registration error – the difference in position after the marker has been registered (reflects the variability of the registration system).
- Target registration error (TRE) - the error in measuring a target once a system is registered.
Of these errors, the most important is the TRE as it determines how confident the surgeon can be when relying on the image guidance.
Smith, et al., (2014) conducted a study whereby they arranged the fiducial markers on a phantom in a number of different arrangements in order to see if the marker placement had an impact on accuracy as measured by the TRE. The arrangements they tested (in addition to 3 random arrangements) were:
- Axial – a band around the head in a coronal plane
- Bifrontal – markers only across the frontal region
- Coronal–sagittal - one line of markers in a single sagittal plane and another in a single coronal plane
- Parasagittal - bilateral lines in parallel sagittal planes
- Two-axis - two different bands around the head in parallel axial planes
- Wide-whole – markers spread across the whole skull
They found that the most accurate arrangement was two axis with a TRE of 1.35 mm +/- 0.065mm. The wide-whole arrangement also performed well (1.43mm +/- 0.061mm) and both performed better than the other arrangements. It is suggested that this is due to the wide distribution of markers in these arrangements which have very little redundancy. This is an important result as it means fiducial marker placement needs to be performed more precisely and taken into consideration when performing or planning a surgery. Particularly since different arrangements may be better in different treatments (West, et al., 2001).
West, et al., (2001) found that for cranial neurosurgery the best approach is to use widely spread fiducial markers as well as placing the markers near to the target. For a different surgery, pedicle screw placement it was found that the best approach was to avoid using collinear markers.
Skull Mounted Trackers (Fanous, et al., 2017)
The first development from frame-based navigation systems was the use of frameless systems based on pre-applied fiducial markers. The problem with marker based registration is that they require additional pre-operative MR images to be taken on the day of the surgery which increases the cost of the surgery. When fiducial markers are used they also require the patients head to be fixed. This re-introduces some of the problems with framed surgeries – namely, it increases the risk of potential skull fractures and limits the surgeons’ flexibility.
To avoid some of these issues facial masks were developed. These do not require pre-operative imaging or fixing of the patient’s head. With a mask based system, a mask with a number of registration points on the face and forehead is applied to the patient. Registration is then performed to the surface of the mask. The disadvantage of the mask-based approach is that the mask prevents a wide sterile field/operating area which is required for certain operations such as the placement of shunts. The mask may also pose an obstacle in surgeries involving the face and forehead.
Electromagnetic (EM) navigation has been successfully used in awake craniotomies. An awake craniotomy is identical to conventional craniotomy in practically every way, except the patient is awake and able to respond to the surgeon during the procedure. This is the preferred neurosurgical technique for operations to remove lesions close to functionally important parts of the brain as it allows the patients neurological function to the tested continuously throughout the operation which reduces the risk of damage to important tissue (University Hospital Southampton, 2014).
Morsy & Ng (2015) found that EM navigation provided the same accuracy as optical navigation with the benefit that the patient did not need to be fixed nor did the surgical tools interfere with the tracking. Considering that the patient is awake for awake craniotomies it is also important that they are as comfortable as possible which is aided by not having their head fixed – the small size of the EM sensor allows free head movement. This is not only advantageous to the patient but also to the surgeon as it means that the head can be rapidly repositioned to allow for airway access and protection if an emergency arises during the procedure.
EM navigation also compared favourable to infrared navigation systems as the sensors (copper coils) can be very small, on the order of several millimetres. In contrast, an infrared (IR) system required a number of emitters and reflectors separated by several centimetres to achieve the same sort of accuracy, thus making IR systems impractical if the patient is not rigidly fixed (Morsy & Ng, 2015).
Surgical Simulators
A surgery simulator is computer technology developed to simulate surgical procedures. This simulators can be used for the purpose of training medical professionals, without the need of a patient, cadaver or animal. They are best suited for two types of skills needed for surgery, eye–hand coordination and the ability to perform three dimensional actions using a two-dimensional screen as a guide. Eye–hand coordination is improved because the simulation can give both visual feedback, by way of a screen, as well as tactile feedback that simulates the manipulation of organs and tissue. Surgical simulators provide a no-risk environment where skills can be gained through harmless repetition.
“Simulators provide harmless and repeatable practice, multiple and varied scenarios, immediate feedback, uniform standards, objective measures, and trend analysis… For neurosurgery, sophisticated simulators would be a great advance in residency training. Although they are very costly, they could be provided in specially designed training centers. Simulators would be highly useful in the certification and maintenance of certification processes as well as in continuing medical education, refreshment of skills, and even surgical rehearsal.”
(Quest, DO. The 2007 AANS presidential address)
What parts does a simulator usually include?
Although simulation environments vary widely in their procedural applications and implementation details, each can be understood in the context of 3 primary components:
graphics/volume rendering,
tissue deformation/model behavior,
and haptic (force) feedback.
Below we discuss all these components one by one as mentioned in (Malone et.al),
- Volume rendering/ graphics :
Computerized 3D volumetric anatomical models are constructed from medical imaging data. The medical imaging techniques that are used can be computed tomography [CT], magnetic resonance imaging [MRI]. The models are constructed through a combination of image processing and geometric modeling. Volume rendering is used to then display these models in the simulation. Below are some of the rendering techniques used,
Direct rendering approaches: These approaches describe an anatomic structure as a volumetric model. This volumetric model is described as cubic elements known as voxels and use image density values to delineate adjacent tissues. Direct rendering produces a true volumetric reflection of original image. This true volumetric reflection comes at a high processing cost, creating a computational burden that may limit the interactive fluidity of simulators.
Indirect rendering, or surface rendering: These techniques generates models that describe only the surface of anatomical structures.These techniques neglect the internal volumetric data. With this the indirect rendering dramatically reduces computational burden and improves the processing speed of medical simulators. Once a structure has been properly segmented from adjacent tissue, it can be assigned appropriate visual and bio-mechanical properties.
Volume rendering: Volume rendering is a labour intensive tasks when used for the purpose of simulation, in particular, in patient-specific models. In addition to that, the real-time integrated processing of tissue behavior and tactile feedback results in a significant computational burden thus remaining an obstacle in the evolution of surgical simulation.
2. Tissue deformation/model behavior :
To facilitate simulation, volume-rendered models must be capable of responding to user manipulation with virtual tissue deformation. Few techniques of handling model behavior are discussed in the section below,
The mass-spring method is a common approach to tissue deformation in real-time simulators. A major limitation of this method, outlined by Spicer.et.al, is its inability to accurately depict a surgical cut.
The finite-element method (FEM) is an approach to tissue deformation that more aptly accounts for tissue bio-mechanics. FEM represents a structure as a lattice of connected 3D volumetric elements, like cubes or tetrahedra. It then uses a variety of mathematical approximation techniques to solve constituent equations that describe the way that a material being modeled responds to applied forces. FEM can produce models with greater bio-mechanical accuracy than those using mass-spring techniques. Thus, FEM enhances the fidelity of tissue deformation, but does so at a high computational cost that may hinder the fluidity of interactive simulators.
3. Haptic feedback:
Haptics, in the context of surgical simulation, broadly refers to the feedback of sensory information. Sensory information includes tactile, kinesthetic, vestibular, and proprioceptive modalities. Haptic feedback is transmitted to the user via a physical interface that interacts with the computer-based graphic model. This is the integration of what is seen with a realistic sensation of what might be felt. i.e mapping what is seen to how it is felt. To produce realistic haptic feedback, simulation environments must be supplemented with external haptic interfaces. These interfaces should be capable of producing accurate tactile sensations.
Minimally invasive neurosurgery have very limited haptic parameters. This makes it most favorable subject for simulation. An endoscopic surgical field can be recreated by a haptic interface that resembles surgery site. Also, by limiting the degrees of freedom of the instruments, they can move above the port. Endoscopic simulator interfaces provide high haptic fidelity without creating a compelling computational burden.
Model building:
Finding and developing suitable models for the purpose of training a neurosurgeon is always a challenge. There is the need for accuracy and realism, and these have to be balanced against cost, rules, and regulations. Model building can be divided into two parts, Algorithmic and Non-Algorithmic. We will delve into the non algorithmic aspects in the section below as discussed in (Waran et.al).
Non algorithmic:
With the 3D printing in the mainstream, it has become possible to create/ print models using the actual patient data. Also using this patient data to aid in the planning of complex surgical procedures as well as to explain such procedures to patients and their relatives. Latest generation of 3D printers allow models to be created out of materials of varying consistency and density thus adding reality to the models created. A brief description of one such study is mentioned below,
A case study from Waren et.al:
The CT data obtained in a patient with a cortically located brain tumor were selected, and the various tissue components (skin, bone, and dura mater as well as the tumor surrounded by normal brain) were segmented.
The 3D printer was able to create various tissue types of varying consistency and density to mimic skin, bone, dura, and tumor (Fig. 13: composite cross-section). In the programming of the machine’s print characteristics to mimic actual tissue handling, a number of features were considered. The “skin” needed to be pliable enough to be cut by a knife and to hold a suture. An interface layer was created to allow the flap to be raised from the underlying “bone” as in a real patient. The “bone” layer was made solid to provide the feel of using conventional perforators and bone cutters.
An interface was also created between the “bone” and “dura,” thus allowing the cranial perforator to stop automatically when the dural layer was encountered.
The “dural” layer was designed to be lifted off the underlying “tumor.” The space occupied by the “tumor” was printed based on the actual patient’s imaging data. This “tumor” was differentiated from the surrounding “brain” by creating a variation in consistency, the “tumor” being softer than the brain. The “tumor” was colored orange, whereas the “brain” was light yellow.
Figure 13 : Cross-sectional view of model with tumor, and drawing delineating parts of the model. Source : Waran et.al
Horizon 2020
EDEN 2020 is part of a funding program by the EU/EC called Horizon 2020. The programme focusses on 3 main areas: basic science, career development and training of researchers and industrial leadership. This last area covers potential solutions to a number of “societal challenges” in different areas such as health, energy, transport, the environment, security and the bioeconomy. The goal for the societal challenges areas in to encourage the implementation of solutions rather than technology development.
Other Projects
In addition to EDEN2020 there are a number of other Horizon 2020 funded projects in a diverse range of areas. A few are summarised below:
- E-ferry (E-Ferry Partners, 2016) is a project that involves the design, building and demonstration of a fully electrically powered car- and passenger ferry so that the overall emission and pollution caused by waterborne transportation can be reduced in the future.
- sCO2-HeRo (The supercritical CO2 Heat Removal System) (sCO2-HeRo Partners, 2016) – A system for reliably and efficiently removing residual heat from nuclear fuel without the need for external power sources. The system aims to be a backup cooling system for reactor cores in case of power loss. Thereby improving the safety of nuclear reactors.
- ChiLTERN (ChiLTERN, 2016) – The ChiLTERN project aims to improve the level of personalised therapy reveived by children with liver cancer. For example, ensuring that each patient receives the right amount of chemotherapy and undergoes the most appropriate surgical procedures. This will be done by assigning patients more accurately to risk groups using genetic tests and biomarkers. Imaging technology tools for planning liver operations in a safer way will also be explored.
- “Click-It” (Click-It Consortium, 2016) – The “Click-It” project aims to improve the use of nuclear imaging to monitor the delivery of nanomedicines. This is currently difficult because most of the nanomedicines are short lived and so difficult to detect using nuclear medical imaging. If longer lasting isotopes are used then the patient receives an unnecessarily high radiation dose. Click-It will develop new tracers to allow for the monitoring of nanomedicines and will test these in canine patients.
Bibliography
Abrishamkar, S. et al., 2011. A New System for Neuronavigation and Stereotactic Biopsy. J Surg Tech Case Report, Volume 3, pp. 87-90.
Agar, N. Y. et al., 2013. Development of Stereotactic Mass Spectrometry for Brain Tumor Surgery. Neurosurgery, 68(2), pp. 280-290.
Barua, N. U. et al., 2013. Robot-guided convection-enhanced delivery of carboplatin for advanced brainstem glioma. Acta Neurochirurgica, 155(8), pp. 1459-1465.
Bilger, A. C. et al., 2017. P14.20 Local control an overall survival after frameless LINAC radiosurgery: a single center experience. Neuro-Oncology, 19(suppl_3), p. iii106.
Bjartmarz, H. & Rehncrona, S., 2007. Comparison of Accuracy and Precision between Frame-Based and Frameless Stereotactic Navigation for Deep Brain Stimulation Electrode Implantation. Stereotactic and Functional Neurosurgery, Volume 85, pp. 235-242.
Bot, M. et al., 2015. Analysis of Stereotactic Accuracy in Patients Undergoing Deep Brain Stimulation Using Nexframe and the Leksell Frame. Stereotactic and Functional Neurosurgery, Volume 93, pp. 316-325.
Breneman, J. C. et al., 2009. Frameless Image-Guided Intracranial Stereotactic Radiosurgery: Clinical Outcomes for Brain Metastases. International Journal of Radiation Oncology, Biology and Physics, 74(3), pp. 702-706.
ChiLTERN, 2016. Children’s Liver Tumour European Research Network, Brussels: European Comission.
Click-It Consortium, 2016. "In Vivo Click PET Imaging Agents”: Improving clinical companion diagnostics, Brussels: European Comission.
Dammers, R. et al., 2008. Safety and efficacy of frameless and frame-based intracranial biopsy techniques. Acta Neurochirurgica, Volume 150, p. 23.
Dorward, N., Paleologos, T., Alberti, O. & Thomas, D., 2002. The advantages of frameless stereotactic biopsy over frame-based biopsy.. British Jounral of Neurosurgery, 16(2), pp. 110-8.
EDEN2020, 2017. EDEN2020 - Objectives, Approach and Impact. [Online] Available at: http://www.eden2020.eu/about/objectives-approach-and-impact/ [Accessed 11 06 2017].
E-Ferry Partners, 2016. E-ferry Report Summary, Brussels: European Comission.
Fanous, A. A. et al., 2017. Frameless and Maskless Stereotactic Navigation with a Skull-Mounted Tracker. World Neurosurgery, Volume 102, pp. 661-667.
Grove, J., 2011. 'Triple miracle' sees huge rise in EU funds for frontier research. London: The Times Higher Education.
Khan, F.R. and Henderson, J.M., 2013. Deep brain stimulation surgical techniques. Handb Clin Neurol, 116, pp.27-37.
Liu, F., Watts, T. & Rodriguez y Baena, F., 2016. Intraoperative GPU-based Surgical Navigation for Needle Steering. GPU Technology Conference, p. Poster.
Lobão, C. A. F., Nogueira, J., Dutra do Souto, A. A. & Antonio de Oliveira, J., 2009. Cerebral biopsy: comparison between frame-based stereotaxy and neuronavigation in an oncology center. Arquivos de Neuro-Psiquiatria, 67(3b), pp. 876-881.
Liu, F., Watts, T. & Rodriguez y Baena, F., 2016. Intraoperative GPU-based Surgical Navigation for Needle Steering. GPU Technology Conference, p. Poster.
Morsy, A. A. & Ng, W. H., 2015. Awake craniotomy using electromagnetic navigation technology without rigid pin fixation. Journal of Clinical Neuroscience, 22(11), pp. 1827-1829.
Murphy, M. J. & Cox, R. S., 1996. The accuracy of dose localization for an image-guided frameless radiosurgery system. Medical Physics, Volume 23, pp. 2043-2049.
Orringer, D. A., Golby, A. & Jolesz, F., 2012. Neuronavigation in the surgical management of brain tumors: current and future trends. Expert Review of Medical Devices, 9(5), pp. 491-500.
Raabe, A., Krishnan, R., Zimmermann, M. & Seifert, V., 2003. Frame-less and frame-based stereotaxy? How to choose the appropriate procedure. Zentralblatt fur Neurochirurgie, 64(1), pp. 1-5.
Radler, J. R., 1993. Apparatus for and method of performing stereotaxic surgery. United States of America, Patent No. US5207223.
Radler, J. R., 2004. Frameless radiosurgery treatment system and method. United States of America, Patent No. US6778850.
Safaee, M., Burke, J. & McDermott, M. W., 2016. Techniques for the Application of Stereotactic Head Frames Based on a 25-Year Experience. Cureus, 8(3), p. E543.
sCO2-HeRo Partners, 2016. sCO2-HeRo Report Summary, Brussels: European Comission.
Sieradzan, K. et al., 2013. ROBOTIC STEREO EEG IN EPILEPSY SURGERY ASSESSMENT. J Neurol Neurosurg Psychiatry, 84(11), pp. E2-E3.
Smith, J. et al., 2008. Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas.. Journal of Clinical Oncology, 26(8), pp. 1338-45.
Smith, J., Quiñones-Hinojosa, A., Barbaro, N. & McDermott, M., 2005. Frame-based stereotactic biopsy remains an important diagnostic tool with distinct advantages over frameless stereotactic biopsy.. Journal of Neuro-oncology, 73(2), pp. 173-9.
Smith, T. R. et al., 2014. Impact of fiducial arrangement and registration sequence on target accuracy using a phantom frameless stereotactic navigation model.. Journal of Clinical Neuroscience, 21(11), pp. 1976-1980.
Uluç, K., Kujoth, G. C. & Baskaya, M. K., 2009. Operating microscopes: past, present, and future. Journal of Neurosurgery, 27(3), p. E4.
University Hospital Southampton, 2014. Awake craniotomy. [Online]
Available at: http://www.uhs.nhs.uk/OurServices/Brainspineandneuromuscular/Neurosurgery/Diagnosisandtreatment/Braintumours/Awakecraniotomy.aspx
[Accessed 17 06 2017].
Varma, T. R. K. & Eldridge, P., 2006. Use of the NeuroMate stereotactic robot in a frameless mode for functional neurosurgery. THE INTERNATIONAL JOURNAL OF MEDICAL ROBOTICS AND COMPUTER ASSISTED SURGERY, Volume 2, pp. 107-113.
Virdyawan, V., Oldfield, M. & Rodriguez y Baena, F., 2016. Laser Doppler Based Sensing for Blood Vessel Detection with a Steerable Needle. 6th Joint Workshop on New Technologies for Computer/Robot Assisted Surgery, p. Presentation.
Wang, D. et al., 2014. Pain experience using conventional versus angled anterior posts during stereotactic head frame placement for radiosurgery.. Journal of Clinical Neuroscience, 21(9), pp. 1538-42.
West, J. B. et al., 2001. Fiducial Point Placement and the Accuracy of Point-based, Rigid Body Registration. Neurosurgery, 48(4), pp. 810-818.
White, T. et al., 2017. Frameless Stereotactic Insertion of Viewsite Brain Access System with Microscope-Mounted Tracking Device for Resection of Deep Brain Lesions: Technical Report. Cureus, 9(2), p. e1012.
Woerdeman, P. A. et al., 2007. Application accuracy in frameless image-guided neurosurgery: a comparison study of three patient-to-image registration methods. Journal of Neurosurgery, 106(6), pp. 1012-1016.
Malone, Hani R., et al. "Simulation in neurosurgery: a review of computer-based simulation environments and their surgical applications." Neurosurgery 67.4 (2010): 1105-1116.
Waran, Vicknes, et al. "Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons: technical note." Journal of neurosurgery 120.2 (2014): 489-492.



















2 Kommentare
Unbekannter Benutzer (ga67yur) sagt:
20. Juni 2017Really nice wiki. The information is detailed but still easy to read which is good. I especially like that you included several examples for future/current developements. As a side note: your figures are not numbered yet but instead there is a "?". Personally I think it would be nice if you include direct links to your sources, but that's just a matter of taste.
All in all great work!
Unbekannter Benutzer (ga39tec) sagt:
20. Juni 2017Your wiki is very detailed and well written. I like your citation-style, too: it results in a very ordered bibliography. Regarding the order/structure of the article: as you have a lot of detail, subpages would help structuring the article and give a better overview of all covered topics.