There are many different options for treating a brain tumor. Decision on which path is followed are based on several factors like
- patient factors: age, health status, medical history; tolerance for medication, procedure, therapies
- tumor factors: type, location and size of the tumor; likelihood of metastases and tumor recurrence
Watchful monitoring
Grade I and II (low-grade) tumors are monitored over time (repeated exams and medical imaging) before any other (if any) treatment is performed.
Surgery [1]
This is usually the first step in any treatment plan in order to
- Obtain a tumor sample for accurate diagnosis
- Remove as much tumor tissue as possible => relieve symptoms or reduce amount of tumor to be treated with radiation or chemotherapy
- Direct access (chemotherapy, radiation implants, or genetic treatment)
- Relieve brain tumor related seizures
Types of surgery
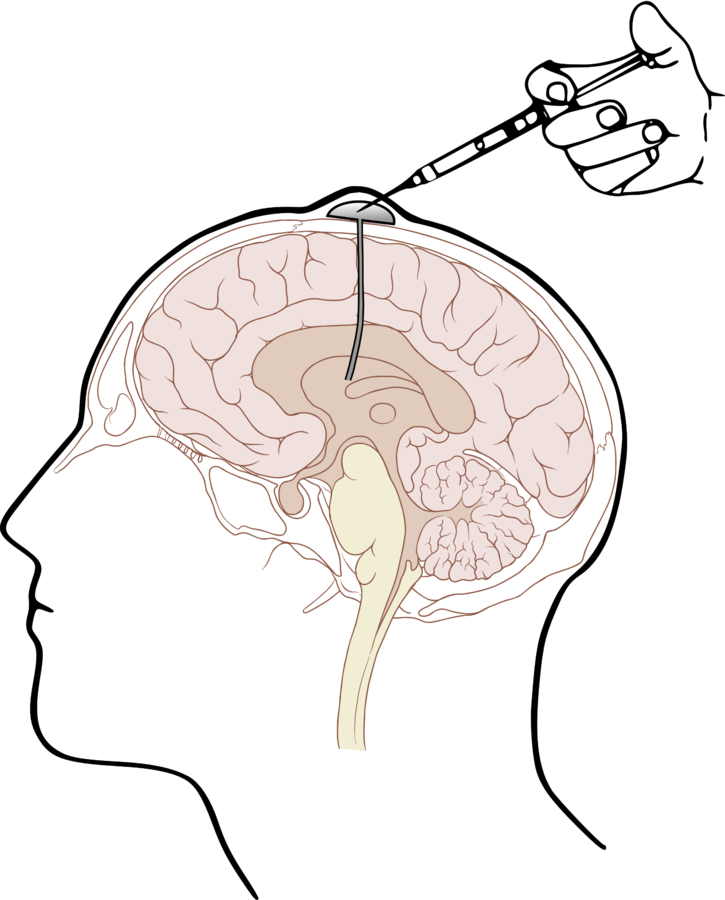
Biopsy
A small tissue sample of the lesion is obtained by drilling a hole in the skull and inserting a needle. This is done under computer-assisted guidance with the help of pre-operative images like MRI or CT. The pathologist examines the sample and decides whether the tumor is benign or malignant. On the basis of the biopsy sample the diagnosis can be verified and improved and therefore a treatment plan can be prepared.
Craniotomy [2]
[2]
In this type of surgery a piece of bone (bone flap) is removed from the skull such that the surgeon can reach the brain and operate on it. After the surgery the bone flap is replaced and fixed with titanium plate and screws
Craniectomy
This procedure is very similiar to craniectomy, but the bone flap is not replaced in order to allow swelling of the brain and to reduce intracranial pressure (ICP)
Partial Removal [3] / Debulking
The tumor volume is decreased as much as possible (usually through surgical removal) to help with following radiation or chemotherapy. This is often a very long and complicated procedure.
Sometimes a tumor is not removed completely to prevent potential damage to nerves or important brain areas.
However, partial removal usually makes sense since it increases effectiveness of other therapies (e.g. radiation). In this regard it is also very important to remove hypoxic (oxygen deficient) tissue, which is resistant to other treatments.
Complete Removal
Some type of tumor sometimes can be removed completely. However, the tumor can potenitially grow back from invisible cells that have been left behind.
Shunt [4,5]
[6]
Used to get rid of excess CSF to reduce ICP. (Plastic) tube where one side is placed in the ventricles and the other in the abdomen. The tube runs under the skin and is controlled by a valve. Instead of the abdomen, the shunt can also be connected to an ommaya reservoir.
Ommaya Reservoir [7]
[6]
This device is a catheter system that connects the ventricles with a reservoir that is implanted under the scalp. It can be used to evaluate free cells in the excess CSF, and to deliver drugs, such as chemotherapeutics or morphine.
What else?
- What type of treatment is used when (stage,grade, type, location of tumor)
- types of craniotomy (http://www.medindia.net/surgicalprocedures/craniotomy.htm , http://www.hopkinsmedicine.org/healthlibrary/test_procedures/neurological/craniotomy_92,P08767/)
- Surgery Risks and Side-Effects (http://neuroinstitute.org/btc/surgery.html)
Radiation therapy [8]
External beam radiation therapy (EBRT)
EBRT direct high-energy radiation beams from outside into the body as close as possible to the tumor location. This destroys cells or inhibitis their growth. Affected healthy cells regenerate faster than tumor cells and thus longer radiation cycles over several weeks are able to kill cancer cells.
The use of protons rather than traditional x-ray or gamma radiation is increasingly researched in many brain tumor types, such as meningiomas [9].
Stereotactic radiation therapy (SRT)
[11]
This procedure is also called gamma knife therapy. It relys on stereotactic headframe support, pre-treatment imaging (CT or MRI) and computer-assisted planning to focus very thin beams of radiation only to the tumor. This procedure is only performed in a single session.
Internal radiation therapy (brachytherapy)
Radioactive implants are placed in and around the tumor.
Chemotherapy [10]
This treatment uses drugs that stop the cancer cells’ ability to grow and divide. The goals are to destroy tumor cells remaining after surgery, slow a tumor’s growth, or reduce symptoms.
The Blood-brain barrier not only keeps harmful substances from entering the brain, but also some chemicals used in chemotherapy when administered intravenously or orally. Options to circumvent this include special chemicals that can pass the blood-brain barrier, dissolvable wafers [15, 16] that can be placed in the space left after surgical removal or more recently catheters that are placed through the skull.
Moldable polymer [14]
Poly(lactic-co-glycolic acid) (PLGA)/poly(ethylene glycol) (PEG) microparticles can be molded around resection cavity and slowly release chemotherapeutic drug, thus working as an adjuvant therapy.
Targeted and Immunotherapy [13]
[17]
Drugs that specifically target molecules, mechanism or pathways in the cells. Such as a monoclonal antibody blocking the protein VEGF (vascular endothelial growth factor) that helps angiogenesis
Steroids [12]
Steroids mainly help with symptom management rather than actual treatment of the tumor itself.
Corticosteroids (produced in a lab, not in the body) help with treating edema that is caused by the tumor, radiation, chemotherapy or surgery
Alternating electric field therapy [18,19, 20]
This therapy is also called Tumor Treating Fields (TTF, TTFields). Although its usage is approved in the USA and Europe (glioblastoma multiforme treatment) the efficacy is greatly debated.
[19]
TTF uses low-intensity electrical fields to disturb cell growth due to dipole alignment of molecules necessary for mitosis, such as those forming the spindle tubules, therefore creating apoptotic cells (dying cells). If the dividing cell has already reached the typical hourglass shape, the electrical field creates a dielectrophoresis effect, directing molecules towards the middle of the cell. This results in uneven distribution of DNA in the daughter cells and thus cell death.
Clinical trials
Clinical Trial Phases [22]
Different stages test different things in a new drug.
Phase 0
Only very few patients take part. This phase test whether a drug behaves the way it is thought to work in human bodies, if it reaches the tumor and how cancer cells respond to it. Usually, doses are too small to cure cancer.
Phase 1
In this phase also only few patients take part and they span a very long time. The trial is not limited to one type of cancer. Administered drug dose is increased over time with more information on patients' reaction to it. This stage tests how much of the drug is safe to give, the occuring side effects, the reaction of the body to it and if tumor size is decreasing.
Phase 2
This stage can, but does not have to be limited to a certain type of cancer. It tests which types of cancer the treatment works for, gives more insights into side effects and their management and the optimal dose.
These trials are typically medium sized (100 patients) and sometimes already compare against standard of care or placebo.
Phase 3
In this phase new treatments are compared to the best available treatment. This can include either a new drug, new doses of the standard treatment or a different way of administering the standard treatment.
The tested cohorts need to be very large to test for small enhancements in results.
Phase 4
After the drug has been granted a licence, a phase 4 trial can follow to find out more about side effects, safety, as well as long term outcomes.
Immunotherapy [21]
6 main areas:
- cancer vaccines
- checkpoint inhibitors
- oncolytic virus therapy
- adoptive cell therapy
- adjuvant immunotherapies
- monoclonal antibodies
Research
Bacteria injection [23, 24]
Intratumoral injection of several different live, attenuated or genetically modified non-pathogenic bacteria species (e.g. Clostridium novyi) has been studied so far, some have even brought it to clinical trials, but never further. The research claims that the bacteria multiply only in tumor and thus inhibit their growth and can also serve as vectors to deliver drugs.
What else?
- When is which therapy used/useful
- Mechanism of steroids
- Advanced, new and experimental treatment options
Targeted therapy - an alternative to chemotherapy?
Bibliography
[1] http://www.abta.org/brain-tumor-treatment/treatments/surgery.html
[2] https://en.wikipedia.org/wiki/Craniotomy
[3] http://neuroinstitute.org/btc/surgery.html
[4] https://www.cancer.org/cancer/brain-spinal-cord-tumors-adults/treating/surgery.html
[5] https://en.wikipedia.org/wiki/Cerebral_shunt
[6] By Cancer Research UK - Original email from CRUK, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=34332972
[7] https://en.wikipedia.org/wiki/Ommaya_reservoir
[8] http://www.texasoncology.com/types-of-cancer/brain-cancer/radiation-therapy-for-brain-tumors
[9] Weber DC, Lomax AJ, Rutz HP, et al. Spot-scanning proton radiation therapy for recurrent, residual and untreated intracranial meningiomas. Radiotherapy Oncology. 2004;71(3):247-9.
[10] http://www.cancer.net/cancer-types/brain-tumor/treatment-options
[11] http://www.aafp.org/afp/2008/1201/p1254.html
[12] Dietrich J, Rao K, Pastorino S, Kesari S. Corticosteroids in brain cancer patients: benefits and pitfalls. Expert review of clinical pharmacology. 2011;4(2):233-242. doi:10.1586/ecp.11.1.
[13] https://www.cancer.org/cancer/brain-spinal-cord-tumors-adults/treating/targeted-therapy.html
[14] Rahman CV, Smith SJ, Morgan PS, et al. Adjuvant Chemotherapy for Brain Tumors Delivered via a Novel Intra-Cavity Moldable Polymer Matrix. Debinski W, ed. PLoS ONE. 2013;8(10):e77435. doi:10.1371/journal.pone.0077435.
[15] Bota DA, Desjardins A, Quinn JA, Affronti ML, Friedman HS. Interstitial chemotherapy with biodegradable BCNU (Gliadel®) wafers in the treatment of malignant gliomas. Therapeutics and Clinical Risk Management. 2007;3(5):707-715.
[16] Wait SD, Prabhu RS, Burri SH, Atkins TG, Asher AL. Polymeric drug delivery for the treatment of glioblastoma. Neuro-Oncology. 2015;17(Suppl 2):ii9-ii23. doi:10.1093/neuonc/nou360.
[17] By Biolprof (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons
[18] https://en.wikipedia.org/wiki/Alternating_electric_field_therapy